MED BLOG
Empowering Seniors Through Neuroscience: Rebuilding Confidence & Independence
Aging often brings physical and cognitive changes that can make everyday activities more challenging. Many seniors may withdraw from hobbies and social interactions they once enjoyed, simply because they no longer feel confident in their abilities. Our neuroscience-based program seeks to change this by equipping seniors with practical tools to rebuild confidence and regain independence.
At the heart of our approach lies neuroplasticity—the brain's remarkable ability to adapt and form new connections. This capability enables the brain to relearn skills that may have been diminished with age.
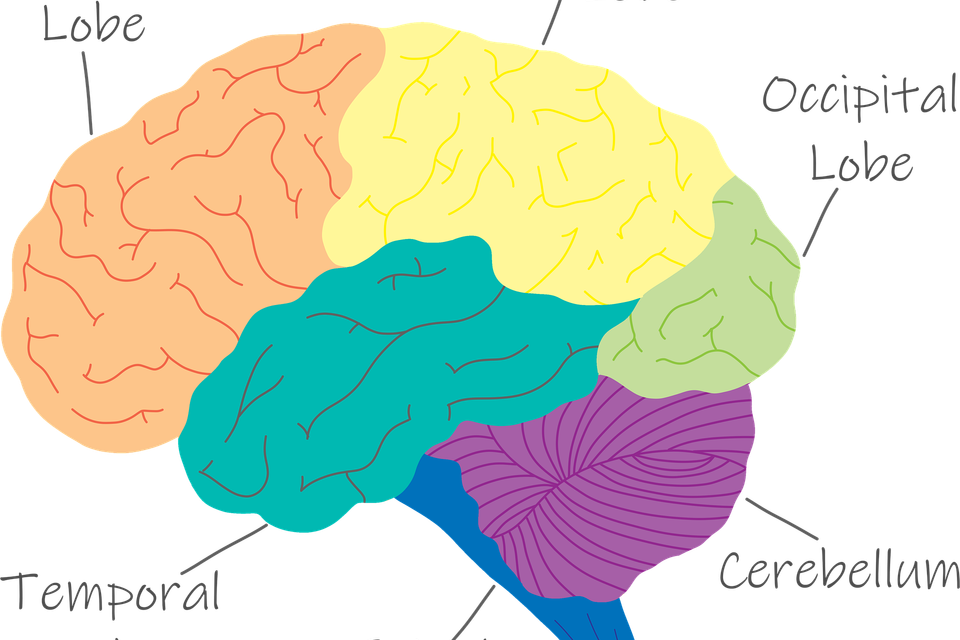
Our program incorporates exercises specifically designed to stimulate the cerebellum, which governs balance, coordination, and other key functions essential for maintaining confidence and independence.
Participation in our program is more than just physical exercise; it’s a cognitive workout that fosters neural growth. With just a few minutes of daily practice, seniors engage in exercises focused on balance, coordination, and cognitive stimulation. These holistic activities are accessible and progressive, helping seniors regain ease in tasks that once felt difficult, eventually making them feel more natural and automatic.
Confidence is a cornerstone of an active lifestyle. When seniors trust in their abilities, they’re more inclined to stay socially engaged, pursue hobbies, and maintain physical activity—all of which contribute to better health and well-being. Our program provides a straightforward path to rediscovering this confidence through consistent, gentle exercises that promote both physical and mental recovery.
Healthcare providers, from chiropractors to senior living facilities, can integrate this program to enhance their clients’ quality of life. By adopting a science-backed approach, you can support seniors in regaining independence while offering measurable improvements tailored to individual needs. The exercises are simple to implement and easily adaptable, making them an excellent addition to any senior care plan.
The program also delivers tangible results. Participants are reassessed every 30 days, offering clear evidence of progress. This feedback not only boosts motivation but also allows for personalized adjustments to keep the exercises appropriately challenging. This dynamic structure ensures ongoing improvement and a sustained sense of achievement.
Are you ready to help seniors rediscover their confidence and independence? Contact us today to learn more about our neuroscience-based, turnkey solution designed to transform senior care.
At the heart of our approach lies neuroplasticity—the brain's remarkable ability to adapt and form new connections. This capability enables the brain to relearn skills that may have been diminished with age.
Our program incorporates exercises specifically designed to stimulate the cerebellum, which governs balance, coordination, and other key functions essential for maintaining confidence and independence.
Participation in our program is more than just physical exercise; it’s a cognitive workout that fosters neural growth. With just a few minutes of daily practice, seniors engage in exercises focused on balance, coordination, and cognitive stimulation. These holistic activities are accessible and progressive, helping seniors regain ease in tasks that once felt difficult, eventually making them feel more natural and automatic.
Confidence is a cornerstone of an active lifestyle. When seniors trust in their abilities, they’re more inclined to stay socially engaged, pursue hobbies, and maintain physical activity—all of which contribute to better health and well-being. Our program provides a straightforward path to rediscovering this confidence through consistent, gentle exercises that promote both physical and mental recovery.
Healthcare providers, from chiropractors to senior living facilities, can integrate this program to enhance their clients’ quality of life. By adopting a science-backed approach, you can support seniors in regaining independence while offering measurable improvements tailored to individual needs. The exercises are simple to implement and easily adaptable, making them an excellent addition to any senior care plan.
The program also delivers tangible results. Participants are reassessed every 30 days, offering clear evidence of progress. This feedback not only boosts motivation but also allows for personalized adjustments to keep the exercises appropriately challenging. This dynamic structure ensures ongoing improvement and a sustained sense of achievement.
Are you ready to help seniors rediscover their confidence and independence? Contact us today to learn more about our neuroscience-based, turnkey solution designed to transform senior care.